Sciatica: Causes and 16 Treatment Approaches
It may be subtle—a slowly increasing level of pain in the buttocks, hip, or leg—or it may hit you so swiftly that it takes your breath away. Sciatica can be excruciating and make even the simplest daily activities challenging. Here’s what you need to know about the causes of sciatica, along with 16 treatment approaches to consider.
What is sciatica?
Many people think of sciatica as a condition, but in truth it is simply the name given to a particular type of pain.
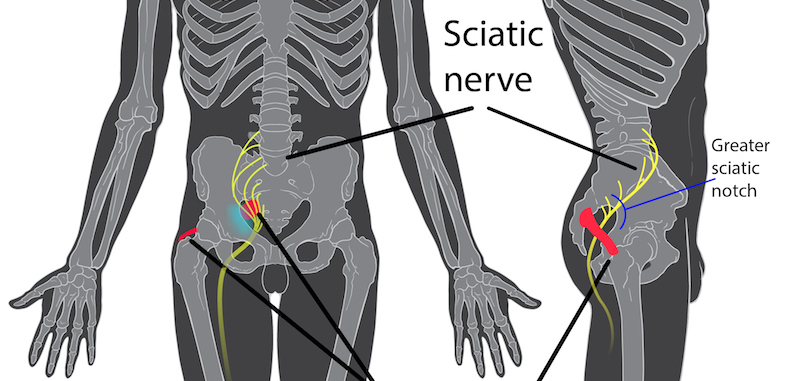
The sciatic nerve is the longest and largest nerve in the body, originating at the lower back, running across the buttock and side of the hip and down the leg before ending at the top of the foot (on both sides of the body). The sciatic nerve controls many of the muscle groups in the lower extremities and provides sensation to the hip, buttocks, thigh, leg, and foot.
When there is injury or trauma to any part of this nerve, sciatic pain can occur. You can see the location of this nerve in the following image.
Sciatica symptoms
Common symptoms of sciatica include:
- Lower back pain
- Radiating pain
- Pain that is burning
- Pain that increases the longer you are in one position (sitting or standing)
- Hip pain
- Tightness in the calf or back of thigh
- Weakness in the lower extremities
- “Pins and needles” feeling along the length of the nerve
- Numbness along the nerve but particularly in the feet and toes
Most symptoms occur on only one side of the body.
Symptoms of serious concern include severe nerve impingement, bladder incontinence, bowel incontinence, lower extremity weakness, and profound loss of sensation.
Loss of bowel or bladder function with sensory deficits and weakness is called cauda equina syndrome. This is a true medical emergency. If this occurs at any point, your should seek immediate medical attention.
What causes sciatica?
Many different conditions can affect the sciatic nerve. In most cases, each condition leads to the sciatic nerve becoming pinched, stretched, or compressed.
Some of the most common causes of sciatica include the following.
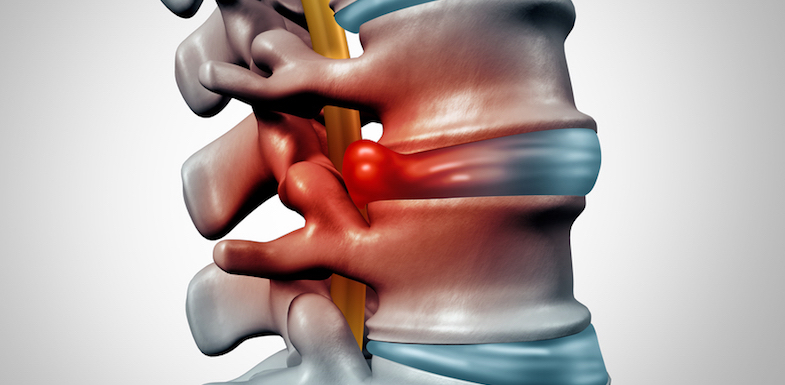
Herniated or bulging disc
This is the most common cause of sciatica.
Separating each vertebra are discs that act as cushions to minimize the impact that the spinal column receives. Since the discs are soft and provide support, over time and with use they can be vulnerable to injury and wear. They may bulge or press through the vertebrae and even break open (herniate).
When this happens, the sciatic nerve can become irritated by pressure or by the disc material itself. Disc issues like these are one of the most common causes of chronic lower back pain and may account for up to 10% of all lower back pain complaints.
Spondylolisthesis
When one vertebra slips over the vertebra below it, the friction that results can cause pain and inflammation in the sciatic nerve.
This condition is called spondylolisthesis.
Spinal stenosis
Spinal stenosis is a narrowing of the spinal canal that causes nerve or spinal cord impingement (pressure or blockage). This condition often results in persistent pain in the lower back and lower extremities. If you have spinal stenosis, you may also experience:
- Difficulty walking
- Decreased sensation in the lower extremities
- Decreased physical activity
Many people with spinal stenosis experience sciatica on both sides of the body.
Osteoporosis
Bones that weaken and thin with age are susceptible to fracture. Osteoporosis is a common cause of sciatic pain.
Some patients may not even realize that they have small fractures in the vertebrae that are irritating their sciatic nerve.
Piriformis syndrome
The piriformis is a large muscle that is part of the pelvis. When this muscle becomes inflamed or overused, this muscle can impinge on or irritate the sciatic nerve deep in the buttock, causing sciatica.
Facet hypertrophy
The facet joints connecting the vertebrae allow for movement, especially towards the back of the body.
When the facet joints become arthritic they can become knobby and large. They also can develop cysts. The larger joints can irritate exiting nerve roots. This irritation and resulting inflammation may result in sciatic pain.
Other sciatica causes
In rare cases, sciatica can also be caused by:
- Tumors
- Pelvic infections
- Injury or trauma to the lumbar spine
Many pregnant individuals also experience sciatica-like symptoms.
How do I get a sciatica diagnosis?
Getting a proper diagnosis of the underlying cause of your sciatica is crucial. While pain symptoms can be treated with medication, if the underlying cause is not treated, further serious complications can occur.
A diagnosis of sciatica is often made after a complete a physical examination that includes a medical history. Your doctor will ask about your symptoms, including:
- When they started
- How long they have lasted
- What affects them (i.e., what types of movement)
It can be helpful to keep track of pain in a journal, mobile pain app, or notebook, so you have ready answers for your doctor during your exam.
Your doctor may also order radiological imaging such as X-ray, CT scan, MRI, or bone scan to uncover potentially serious conditions such as cancer or broken bones. If you have a history of cancer, IV drug use, HIV infection, or recent steroid use, your doctor will be more inclined to order extensive lab tests to uncover the root cause of your pain.
16 sciatica treatments
If there is any good news when it comes to sciatica, it’s that there are a number of treatments that can safely and effectively treat your pain and other symptoms. In many cases, non-invasive sciatica treatments provide relief without more complicated interventions.
Here are 16 sciatica treatment options to consider.
- Nutrition and exercise
- Biofeedback
- Physical therapy
- Deep tissue massage
- Acupuncture
- Medications
- Transcutaneous electrical stimulation (TENs)
- Epidural steroid injections (ESI)
- Trigger point injections (TPIs)
- Infusions
- Lysis of adhesions
- Disc decompression
- Spinal cord stimulation (SCS)
- Intrathecal pump implants
- Percutaneous discectomy
Always work closely with your doctor, following their advice for treatment.
Nutrition and exercise
Exercise can reduce the pain of sciatica by increasing flexibility and range of motion. Another benefit of regular exercise is the release of hormones called endorphins, which are your body’s natural pain relievers. Yoga and Pilates are both good introductory practices you can modify to your comfort level.
Nutrition and healthy eating are powerful treatments that combat nutritional deficits and control inflammation. In combination with one another, changes to diet and exercise can offer profound sciatic pain relief.
Biofeedback
This is a treatment that teaches you how to become aware of involuntary processes inside of the body (such as blood pressure, temperature, and heart rate control).
This method enables you to gain some conscious control of these processes, which can influence and improve your level of pain. A better awareness of one’s body teaches one to effectively relax, which can help to relieve pain.
Physical therapy
Physical therapy helps improve symptoms of sciatica by increasing flexibility, range of motion, posture, while also improving muscle strength.
This type of therapy is an excellent treatment approach when done alongside other complementary treatments. For example, you may take pain-relieving medications for short-term pain while also undergoing physical therapy to resolve the underlying cause of your sciatica.
Deep tissue massage
Sciatic massage of tender areas may help relieve muscle spasms or contractions and improve the discomfort associated with it.
Massage as a sciatica therapy can also help you relax, decreasing stress and tension.
Acupuncture
With this ancient Chinese therapy, small needles are inserted into your skin. These needles cause your body to release hormones called endorphins, which are your body’s natural pain relievers.
Acupuncture can also help you relax, decreasing stress, tension, and muscle spasms.
Medications
NSAIDs (ibuprofen-like drugs), acetaminophen, membrane-stabilizing drugs, muscle relaxants, and other analgesics are often used in the management of pain associated with sciatica.
It is important to note that there is no evidence that opioid treatment is effective for sciatica.
Transcutaneous electrical stimulation (TENs)
This pain relief technique is a passive process with no known side effects. Your doctor places patches on your skin in the affected area. These patches deliver a mild electrical current that interrupts the pain signals to the brain. A tingling sensation replaces those pain signals that typically reach your brain.
TENs unit therapy may help to:
- Reduce your perception of pain
- Relax your muscles
- Improve mobility
Epidural steroid injections (ESI)
This procedure involves injecting a medication into the epidural space where the actual irritated nerve root is located.
This injection includes both a long-lasting steroid and a local anesthetic (lidocaine). The steroid reduces the inflammation and irritation and the anesthetic works to interrupt the pain-spasm cycle and nociceptor (pain signal). The combination medicine then spreads to other areas of the spine, reducing inflammation and irritation.
This sciatica treatment usually takes less than 15 minutes. The biggest benefit to this treatment is the rapid relief patients often experience. While this relief is temporary, it can allow them to begin other treatments, such as exercise and physical therapy, that they were unable to do before.
Watch the following video to learn more about this procedure.
Trigger point injections (TPIs)
These can be an effective treatment for muscle spasms that lead to sciatica.
The procedure involves injecting a local anesthetic and steroid into a trigger point. Performing a piriformis injection can be considered a type of TPI.
Infusion techniques
This procedure involves inserting a small catheter through a needle into the epidural space or directly next to affected nerves.
Local anesthetic and other medicines are often given through the catheter for extended time periods. When the nerves are blocked continuously with an infusion, pain relief can be dramatic and long-lasting.
Lysis of adhesions
Also known as the “Racz procedure,” this sciatica therapy can help remove excessive scar tissue in the epidural space. It’s also another pain relief option when other conservative treatments have failed.
A study performed in 2005 noted that:
“Spinal adhesiolysis with targeted delivery of local anesthetic and steroid is an effective treatment in a significant number of patients with chronic low back and lower extremity pain without major adverse effects.”
Disc decompression
With this procedure, a needle is inserted through the skin into the affected disc. Disc material is suctioned out of the bulging disc and pressure is relieved within the disc.
This treatment is best combined with strengthening exercises to prevent further injury.
Spinal cord stimulation (SCS)
For this sciatica treatment, an implanted electrical device can decrease the perception of pain by interrupting pain signals being sent to your brain. Your doctor will perform a short trial procedure to see if this device will help you long-term.
In the initial trial, your pain physician places a small electrical lead through a needle in the epidural space. A tingling sensation will replace your pain signals. If this does manage your pain, you may opt to have your doctor implant a permanent SCS device.
Intrathecal pump implants
Implanted pain pumps are also available. These can be extremely helpful at providing long-term pain control.
These pumps deliver medication that can include local anesthetics or muscle relaxants in regular intervals to a specific area in the body.
Percutaneous discectomy
This procedure can help treat bulging or herniated discs that are pressing on the sciatic nerve. Heat or radio waves remove ruptured disc material to reduce the size of the disc.
Many patients feel immediate relief from pain after removal of the material compressing the nerve. Watch the following video to learn more about this procedure.
References
- Rheumatology (Oxford). 2005 Nov;44(11):1399-406. Epub 2005 Jul 19 Arden NK, Price C, Reading I, Stubbing J, Hazelgrove J, Dunne C, Michel M, Rogers P, Cooper C; WEST Study Group. Rheumatology (Oxford). 2005 Nov;44(11):1399-406. Epub 2005 Jul 19 PMID: 16030082
- Interventional Techniques: Evidence-based Practice Guidelines in the Management of Chronic Spinal Pain. Boswell et. All. Pain Physician 2007; 10:7-111