Imagine a condition where brushing a stray hair off of your cheek causes excruciating and debilitating pain, pain that is unresponsive to pain medication and lasts long after the light touch has stopped. This is a brief glimpse into the mysterious pain of trigeminal neuralgia. Understanding what causes trigeminal neuralgia can lead to a proper diagnosis and successful treatment of pain. Here’s what you need to know.
What is trigeminal neuralgia?
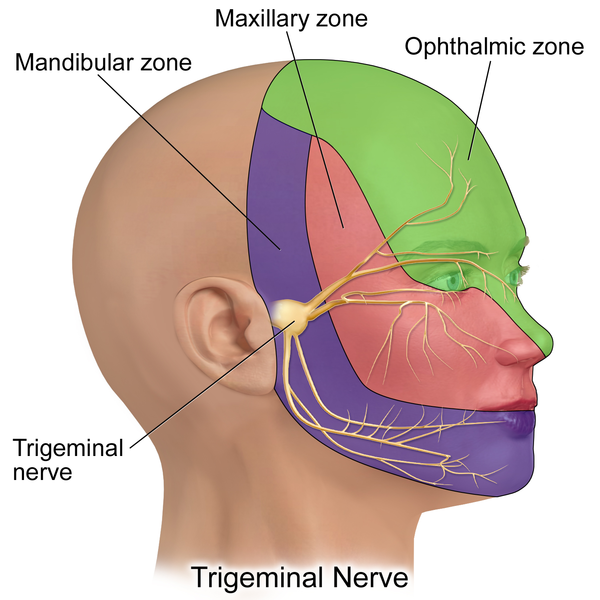
Trigeminal neuralgia is a type of neuropathic (nerve related) pain that stems from the trigeminal nerve. This nerve has three branches that bring sensation to different parts of the face. These include:
- Upper: Controls sensation in the eye, upper eyelid, and forehead
- Medial: Sensation control in the lower eyelid, cheek, nostril, upper lip, and upper gum
- Lower: Responsible for feeling in the jaw, lower lip, lower gum, and inside the mouth
Each branch originates between the end of the lower jawbone and the ear, right where the temporomandibular joint comes together. Trigeminal neuralgia pain is most often felt on one side of the face but can occur bilaterally (on both sides) as well.
Atypical trigeminal neuralgia includes a variety of other symptoms and may coincide with overlapping conditions, such as temporomandibular joint disorder.
An estimated 150,000 people in the U.S. receive a trigeminal neuralgia diagnosis each year. Commonly misdiagnosed as migraine, trigeminal neuralgia may, in fact, affect many more people than previously thought.
Do I have trigeminal neuralgia?
In the early stages of trigeminal neuralgia, trigeminal neuralgia symptoms may be sporadic and fleeting. Because there is no regularity to them, patients may not seek immediate treatment. Shooting pain and spontaneous pain not traced to a particular cause may be the first symptoms that occur. They may disappear as suddenly as they arrive, making a person believe the pain was caused by something episodic (e.g., a sudden movement or slight injury).
Other early trigeminal neuralgia symptoms may include:
- Ear pain
- Nausea
- Fatigue
- Sensitivity to light
These are similar to symptoms experienced by migraine sufferers and may lead to an incorrect diagnosis. When symptoms are treated as migraine pain, they will continue and worsen.
As symptoms get worse, patients may experience episodic pain. This occurs with increasing regularity as patients endure an intense period of pain followed by remission. As nerve damage worsens, so does the pain and periods of remission get shorter.
In some cases, patients begin to experience a constant ache or burning sensation. For patients who do not experience a constant dull ache, increasingly frequent attacks occur. This pain will be unresponsive to any type of pain medication and is uneven in its duration.
Symptoms are different in their onset, severity, and response to treatment from patient to patient due to the cause of the pain and any comorbid conditions that might complicate an accurate diagnosis.
What causes trigeminal neuralgia?
Trigeminal neuralgia is challenging to diagnose because no one thing causes pain 100% of the time in every patient. A potential cause in one person may not produce any pain in another.
However, here are some of the more common trigeminal neuralgia causes:
- Damage to the trigeminal nerve: Any kind of blow or injury to the jaw can potentially damage the trigeminal nerve. This damage can cause excruciating pain while the injury heals.
- Nerve compression: Nerve compression caused by a tumor or other mass of tissue is not the most common cause but does occur in some patients. Tumors can be benign and still press on the nerve, causing pain.
- Multiple sclerosis: Multiple sclerosis causes damage to the myelin sheath, the protective coating on the trigeminal nerve. Once this sheath is compromised or worn, exposing the nerve, pain can occur.
- Scleroderma: Scleroderma is a very rare chronic connective tissue disorder that is classified as an autoimmune condition. Among other symptoms, trigeminal pain can occur in later stages.
- Shingles (herpes zoster): Shingles is a viral infection of the nerves. Common symptoms include a raised, painful rash and, less typically, trigeminal neuralgia pain. Trigeminal pain generally occurs when the shingles rash in located near or on the head, face, or neck.
- Deformity in the arteries and veins: Tangled arteries and veins that become swollen with blood can compress the trigeminal nerve.
What are trigeminal neuralgia risk factors?
Age and gender are primary risk factors, as women over the age of 50 are most likely to develop this condition. Hypertension (high blood pressure) is also a risk factor, as is the occurrence of a stroke.
Excessive or improper dental work can cause neuropathic facial pain, as can surgery on the sinuses.
Finally, any blow or injury to the face (i.e., as a result of a contact sport injury) is a risk factor for trigeminal neuralgia.
What causes trigeminal neuralgia to flare up?
One of the most challenging aspects of trigeminal neuralgia is how sensitive the pain response becomes. Even the lightest stimulation of the painful area can produce lightning bolts of pain across the face.
Some common trigeminal neuralgia triggers include:
- Shaving
- Touching your face
- Eating
- Drinking
- Brushing your teeth
- Talking
- Putting on makeup
- A breeze on the face
- Rising or falling barometer
- Showering
- Smiling (or frowning)
- Increase in blood pressure
- Cold weather
- Drinking alcohol
- Stress
- Washing your face
Oral surgeries and even a regular dental cleaning can also be major triggers, causing some patients to neglect their oral health.
Based on this list of major pain triggers, it is easy to see how trigeminal neuralgia can become debilitating, make everyday life excruciatingly painful.
How to treat my pain
It is important to understand that traditional pain treatments are generally ineffective for this type of neuropathic pain. Why this is so is not well understood, but it is one of the main reasons that people suffering from trigeminal neuralgia can feel hopeless about treatment.
Proper diagnosis is key, however, and there are treatment options that can help you manage and reduce your symptoms.
Trigeminal neuralgia diagnosis
Due to the debilitating severity of pain and its accompanying symptoms, trigeminal neuralgia is sometimes referred to as the suicide disease. Patients who experience this condition have a higher rate of suicide and a greater risk of depression and anxiety. Getting a proper diagnosis is key to treating this disease, and it starts with a complete medical history, including identifying any risk factors.
Other conditions such as temporomandibular joint disorder, cluster headaches, migraine, and post herpetic neuralgia will be ruled out first. In some cases, an MRI looks for tumors pressing on the trigeminal nerve.
Your doctor will also rule out any issues with the sinus cavity, eye conditions, or psychologic disorders. Essentially, absent a visible tumor pressing on the nerve, the process of elimination is what leads to a proper diagnosis.
In some cases, a short course of tricyclic antidepressants or anticonvulsant medication may be administered. If pain responds to these treatments, that may lead to a diagnosis of trigeminal neuralgia.
Trigeminal neuralgia treatments
Trigeminal neuralgia treatments begin most often with medication, but not pain medication. Both over-the-counter and prescription pain medications produce little if any pain relief and are more associated with side effects than analgesic effects. Three types of prescription medications instead – anticonvulsants, antidepressants, and muscle relaxants – are the first line of pharmacological defense for trigeminal neuralgia.
Anticonvulsant options include the following four medications.

1. Carbamazepine
The most common medication for treating trigeminal neuralgia, carbamazepine can help with pain in the earliest stages of trigeminal neuralgia. This medication is also used as a diagnostic test. If carbamazepine relieves pain when administered over a short period of time, this may be a sign of trigeminal neuralgia.
This medication is most effective in the early stages of trigeminal neuralgia, and its effectiveness decreases over time.
2. Phenytoin
Phenytoin is the first medication designed to treat trigeminal neuralgia. Note that there are side effects that may include gum overgrowth, balance issues, and drowsiness.
3. Oxcarbazepine
Oxcarbazepine is a cousin of carbamazepine but comes with fewer side effects. Although patients may experience dizziness and double vision, these side effects are usually mild and manageable.
4. Gabapentin
Gabapentin is an anticonvulsant that is also prescribed for anxiety, restless leg syndrome, and withdrawal from some types of drugs and alcohol. Side effects of this medication include increased hostility, motion sickness, and blurred vision.
Antidepressants
Antidepressants are also commonly used to treat trigeminal neuralgia (although the mechanisms behind how they work is not entirely clear).
Tricyclic antidepressants such as amitriptyline or nortriptyline may successfully reduce or eliminate painful outbreaks. They can also help relieve other related symptoms.
If medication does not relieve pain, more interventional approaches may be needed.
Interventional approaches
If the cause of your trigeminal pain is compression of the nerve, microvascular decompression may help. The microvascular decompression procedure identifies the blood vessel applying pressure and moves it away from the trigeminal nerve. This can decrease nerve sensitivity and give the trigeminal nerve the space it needs to repair itself.
While microvascular decompression can be remarkably effective, opening the skull to perform it comes with substantial risk, including facial numbness and weakness and potential hearing loss.
Lesioning techniques is another category of surgical intervention that can help relieve pain. These include:
- Percutaneous stereotactic rhizotomy: Percutaneous stereotactic rhizotomy uses heat that passes through an electrode and into the trigeminal nerve to destroy the pain-causing part of the nerve and block pain signals to the brain
- Percutaneous glycerol rhizotomy: Glycerol performs the same function as heat to block pain signal transmission to the brain
- Stereotactic radiosurgery (also known as gamma knife): A pinpointed dose of ionizing radiation to the trigeminal nerve roots causes a pain-blocking lesion to form
- Percutaneous balloon compression: A small balloon is temporarily placed in the trigeminal nerve itself, inflated to destroy pain-causing fibers within the nerve
The above lesioning techniques are less invasive than an open surgery, but the effects may not be permanent. All surgeries come with risks, and lesioning techniques are no different. Side effects and risks include lingering soreness, nerve damage, or infection.
Even if pain relief is not as long-lasting, lesioning techniques may be best for patients who are in otherwise poor health, suffer from severe pain, and cannot tolerate a more invasive procedure.
Other treatment options
Experimental treatments using sodium channel blockers are also having some success in treating trigeminal neuralgia related to multiple sclerosis, but this research is in its infancy.
Complementary approaches including biofeedback, firm facial massage (as tolerated), mindful meditation, and acupuncture may also help relieve the pain of trigeminal neuralgia.
If you have more questions about what cause trigeminal neuralgia and how to treat it, get in touch with Arizona Pain today. Our gentle, compassionate doctors can answer your questions and help you get your life back!
